When I meet a new patient I spend 90 minutes with them, piecing together an extensive timeline, working decade by decade to create a thorough personal history, both generational and environmental. It’s the first step in developing a holistic view of the patient. The next step is testing – looking for the normal, the abnormal, and the path toward prolonged health and vital aging.
This year, I expanded my offerings to include new methods of health assessment, bringing in high-tech tools that screen for and monitor biomarkers of health and risk of disease. In the weeks to come, I will be sharing information on the office’s new technology. I hope that you, too, will recognize the importance of wellness through prevention and not wait until you are “sick enough” to take steps toward living optimally.
Body Composition

Research on fat percentage as an indicator of overall health is improving, and studies show that Body Composition Analysis is emerging as a better predictor of disease risk than Body Mass Index (BMI). Body Composition Analysis is a non-invasive method of accurately reporting body fat (including visceral fat), lean muscle mass, basal metabolic rate and total body water. The analysis is helpful in its predictive value regarding cardiovascular disease, metabolic syndrome conditions such as diabetes and insulin resistance and cancer.
The biggest advantage for me as a practitioner is the ability to measure visceral fat and lean muscle mass. Visceral fat is strongly associated with many of the chronic diseases that commonly plague us, including metabolic syndrome, cardiovascular disease, non-alcoholic fatty liver, diabetes and breast, prostate and colon cancers. Visceral fat is stored deep in the abdominal cavity near and around many vital organs, different from subcutaneous fat (the fat you can pinch), and thought to be more biologically active and secrete inflammatory mediators. The ability to accurately identify the presence of visceral fat will assist in the management of:
- Cancers
- Cardiometabolic Disease
- Aging and Longevity
- Liver Health
- Gastrointestinal Health
- Brain
- Eye Health
- Urologic/Kidney Health
- Bone Health
Recently I suggested a Body Composition Analysis to one of my patients who has been struggling to gain some improvement in her bone density. She is a normal weight 64-year-old woman who works out regularly, including using weights three times a week. The Body Composition Analysis showed that despite having a “normal” BMI, her body fat percentage is high and her lean muscle is low. This has been called “skinny fat” or is known as sarcopenia obesity. Using the analysis of her extremities, we can now guide her in a new exercise regimen that will help to gain muscle mass.
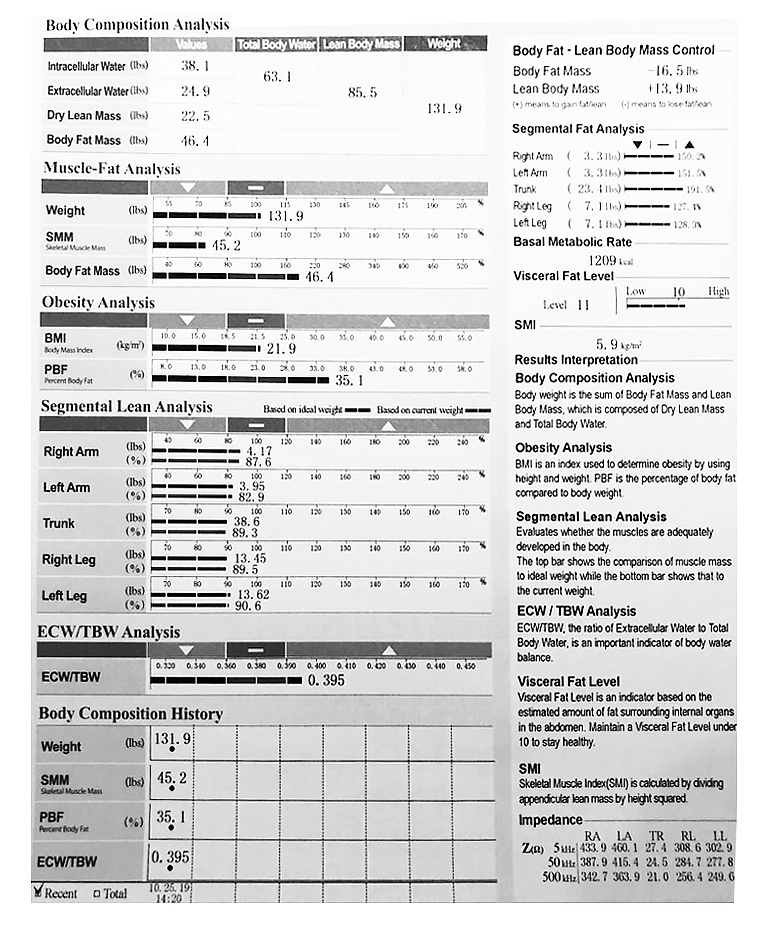
My patient’s willingness to share her case offers a good example of the benefits of completing a baseline Body Composition Analysis. The reading not only reveals much about a patient’s current health, but also allows physicians to predict risk and track changes that can aid patients in education and early detection of disease, as well as setting and achieving goals for diet and exercise.
Worth Reading
Baltadjiev AG, Assessment of body composition of male patients with type 2 diabetes by bioelectrical impedance analysis, PubMed.gov/NCBI/2011
Benbow, Julia M., Choi, Seul Ki, Deal, Allison Mary, et al., Differences in body composition between patients with early or metastatic breast cancer, Journal of Clinical Oncology/2017
Buist, Nicole, de Kruif, Anja Th. C. M., Geenen, Maud, et al., Body composition is associated with risk of toxicity-induced modifications of treatment in women with stage I–IIIB breast cancer receiving chemotherapy, Breast Cancer Research and Treatment/CrossMark/2018
Dannenberg, Andrew, High Body Fat Increases Breast Cancer Risk for Women with Normal BMI, Weill Cornell Medicine/2018
DePolo, Jamie, BMI Not Best Measure of Body Fat When Estimating Breast Cancer Risk in Postmenopausal Women, JAMA Oncology/2018
Harvard Medical School, Abdominal fat and what to do about it, Harvard Health Publishing/2019


